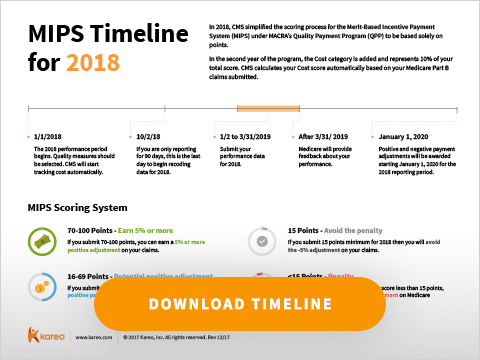
2018 MIPS Timeline and Scoring System
In 2018, CMS simplified the scoring process for the Merit-Based Incentive Payment System (MIPS) under MACRA’s Quality Payment Program (QPP) to be based solely on points.
Under MIPS, providers’ Medicare reimbursements will be adjusted up or down based on how they score across four categories:
- Quality
- Advancing Care Information
- Improvement Activity
- Cost
In the second year of the program, the Cost category has been added and represents 10% of your total score. CMS calculates the Cost score automatically using administrative claims data, if clinicians meet the case minimum of attributed patients. MIPS performance is compared against performance of other eligible clinicians and groups during the performance period, so the benchmark is not based on a previous year.
Here’s the breakdown of the four categories:

And here is a helpful table provided by the CMS, showing final scores and their correlating payment adjustment for 2017 and 2018.

As you can see, the penalty for low to no participation is increasing. Eligible clinicians are encouraged to start the reporting process now. Here’s a graphic that shows the main milestones to remember for this year’s MIPS participation, as well as an explanation of the new scoring system:
MIPS Timeline for 2018 (click to download)